A Skeptical Approach to Mesenteric Ischemia
Fatih Öztürk*, Ali Kemal Gür, Rabia Çoldur, Mustafa Tuncer
DOI10.36648/2471-8157.21.7.148
Fatih Öztürk1*, Ali Kemal Gür2, Rabia Çoldur1, Mustafa Tuncer1
1Department of Cardiology, Van YYU Dursun OdabaÅ? Medicine Center, Turkey
2Department of Cardiovascular Surgery, Van YYU Dursun OdabaÅ? Medicine Center, Turkey
- *Corresponding Author:
- Öztürk F
Department of Cardiology
Van YYU Dursun OdabaÅ? Medicine Center, Turkey
E-mail: fatihozturk2488@gmail.com
Received Date: July 18, 2021; Accepted Date: September 10, 2021; Published Date: September 18, 2021
Citation: Öztürk F, Gür AK, Çoldur R, Tuncer M (2021) A Skeptical Approach to Mesenteric Ischemia. Interv Cardiol J Vol.7 No.9:148.
Introduction
Median arcuate ligament (MAL) is a fibrous band that generally encircles the aorta at the level of the first lumbar vertebra, superior the coeliac truncus and connects the diaphragmatic crus. In 10%-24% of people the ligament may cross proximal of coeliac truncus, it rarely reduces the blood flow and causes the symptoms [1]. This syndrome generally occurs in young women and nonspecific symptoms make difficult to diagnose [2]. Common symptoms are especially postprandial epigastric pain, weight loss, nausea, vomiting, abdominal bloating and food fear; also the pain is often on expiration [3]. This case is called as median arcuate ligament syndrome (MALS) and also known as celiac artery compression syndrome or Dunbar syndrome [4].
Case Report
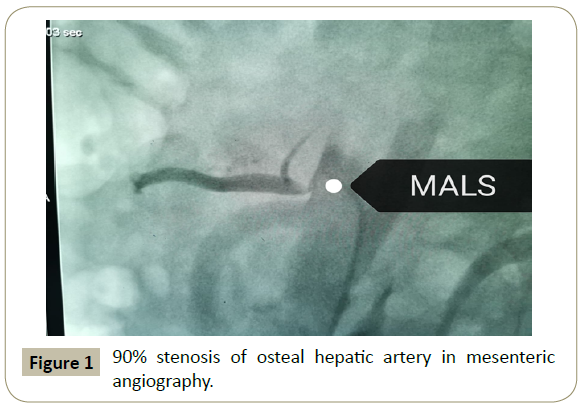
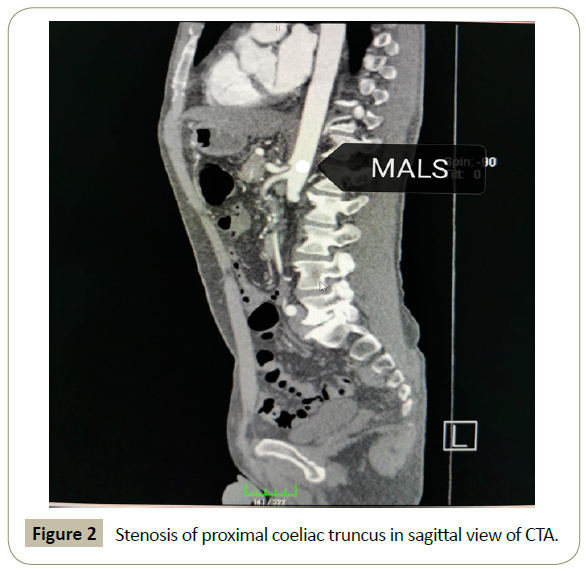
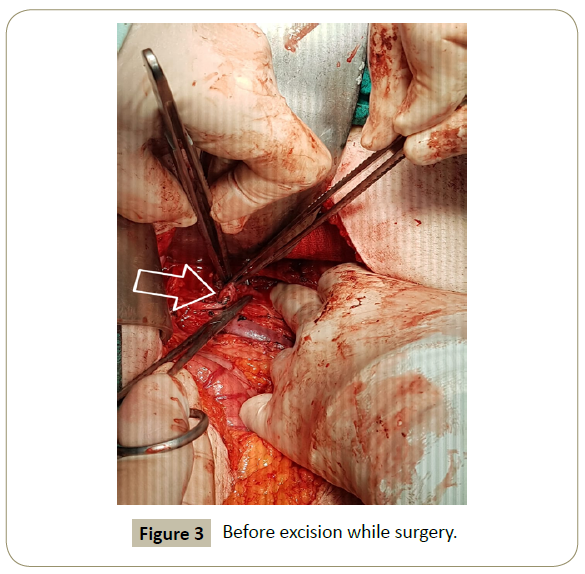
A 54 year-old man presented at the various clinics with chronic postprandial epigastric pain lasting a few hours for 7 months. Esophagogastroduodenoscopy (EGD) showed pangastritis. Abdominal CTA revealed 80%-90% stenosis of the proximal coeliac truncus and the patient was sent to our clinic to perform mesenteric angiography. His physical examination was unremarkable. His fever was 36.5 degree Celsius, blood pressure was 100/60 mmHg, heart rate was 90 beats/min, ECG was normal sinus rhythm, abdomen was normal and Traube’s space was open. Mesenteric angiography being performed in our clinic revealed 90% stenosis of the osteal hepatic artery (Figure 1). Repeated CTA revealed that median arcuate ligament encircled the proximal coeliac truncus and caused an obstruction (Figure 2). The patient underwent open surgery to release median arcuate ligament on coeliac artery (Figure 3).
Discussion
In the differential diagnosis of nonspecific abdominal pain, mesenteric ischemia is one of the first diagnoses that come to mind [5]. The physicians dealing with vascular invasive intervention should evaluate the lesions with clinical experiences and have skeptical approach. The main treatments of MALS are endovascular intervention, open surgery (intraperitoneal and retroperitoneal), robotic and laparoscopic surgery, coeliac ganglionectomy and percutaneous coeliac plexus blockade [6]. Our case recuperated with open surgery.
Conclusion
As in our case, typical lesions (trombus, nonocclusive lesion or embolism) were not observed in angiography of the patient with mesenteric ischemic prediagnosis, it brought to mind the diagnosis of MALS. To ensure the diagnosis before interfering the stenosis, CTA was repeated and the diagnosis was confirmed. Otherwise, if we interfered with the stenosis percutaneous, it would be impossible to open the stent where the ligament encircled and be iatrogenically embolized or the procedure would result in complication like vascular injury that we could not even think. We want to emphasize with our case that MALS should be brought to mind when interfering mesenteric arteries.
References
- Andrew JD, Panait L, Eisenberg D, Robert LB, Roberts EK, et al. (2009) Management of median arcuate ligament syndrome: a new paradigm. Annals of vasc sur 23: 778-784.
- Goodall R, Langridge B, Onida S, Ellis M, Lane T, et al.(2019) Median arcuate ligament syndrome. J Vasc Surg 71: 2170-2176.
- Wolfman, D., E.I. Bluth, and J. Sossaman (2003) Median arcuate ligament syndrome. J Ultrasound in Med 22: 1377-1380.
- Dunbar JD, Molnar W, Beman FF, Marable SA (1965) Compression of the celiac trunk and abdominal angina: preliminary report of 15 cases. Am J Roentgenol 95: 731-744.
- Yanar F, Agcaoglu O, Sarici IS, Sivrikoz E, Ucar A, et al. (2013) Local thrombolytic therapy in acute mesenteric ischemia. World J Emer Sur 8: 8.
- El-Hayek KM, Titus J, Bui A, Mastracci T, Kroh M (2013) Laparoscopic median arcuate ligament release: are we improving symptoms. J Am Col Sur 216: 272-279.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences